Hair loss, medically known as alopecia, is a common concern affecting millions worldwide. While often perceived as a purely cosmetic issue or an inevitable sign of aging, it can frequently be a significant indicator of underlying health problems. Far from being a superficial complaint, hair loss can signal a range of internal imbalances, nutritional deficiencies, autoimmune disorders, or chronic illnesses that warrant medical attention. Understanding the intricate connection between hair health and overall well-being is crucial for accurate diagnosis and effective treatment.
This article delves into the various health conditions that can manifest as hair loss, emphasizing why a thorough medical evaluation is essential when experiencing unexplained or excessive shedding.
The Hair Growth Cycle and Its Disruptions
To understand hair loss, it’s helpful to briefly review the hair growth cycle. Each hair follicle goes through three main phases:
- Anagen (Growth Phase): Lasts 2-7 years, with hair actively growing.
- Catagen (Transition Phase): Lasts 2-3 weeks, hair growth stops.
- Telogen (Resting Phase): Lasts 2-4 months, old hair rests while new hair begins the growth phase. At the end of telogen, the old hair sheds.
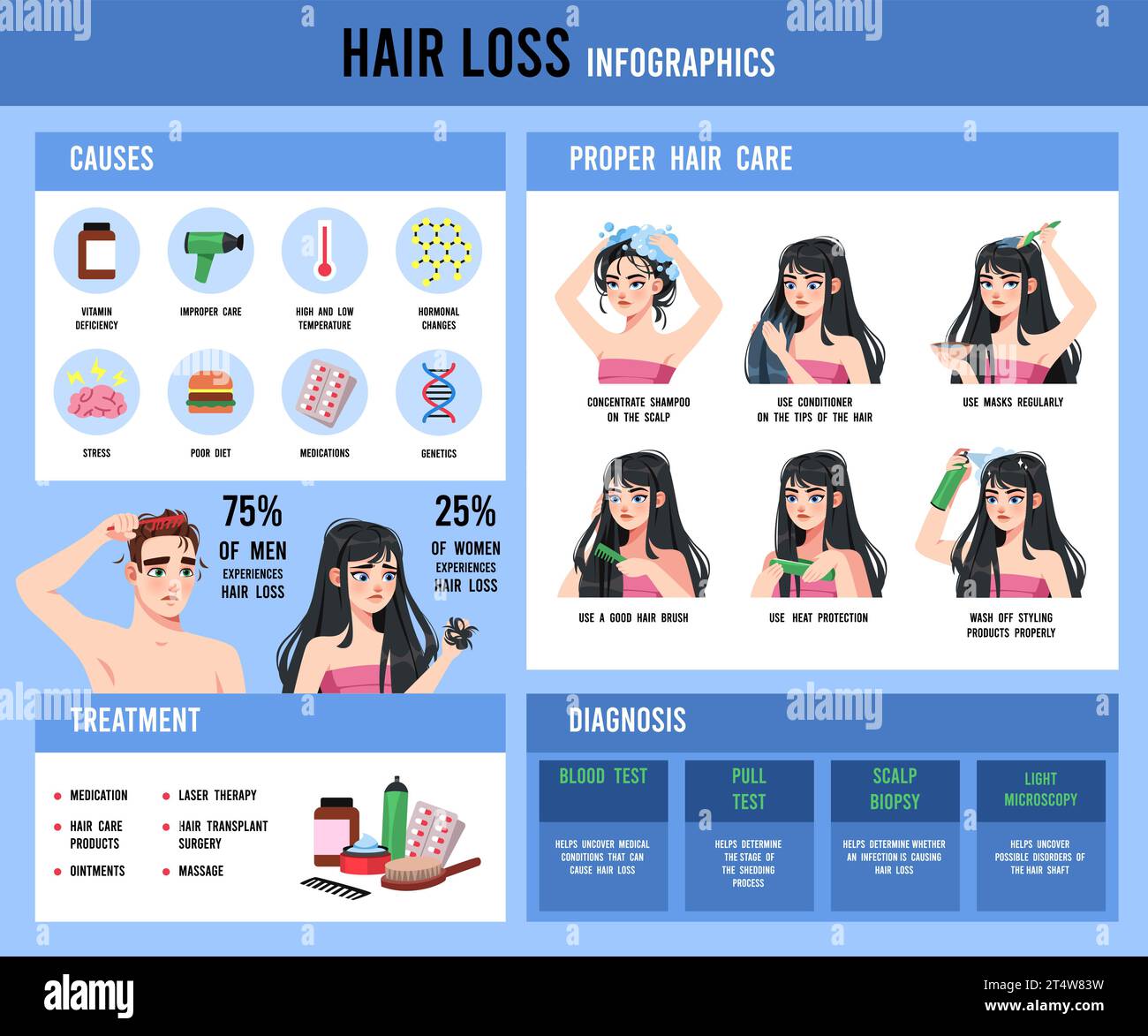
Disruptions to this cycle can lead to various forms of hair loss. The most common types include:
- Androgenetic Alopecia (Pattern Baldness): A genetic predisposition influenced by hormones, leading to a predictable pattern of thinning.
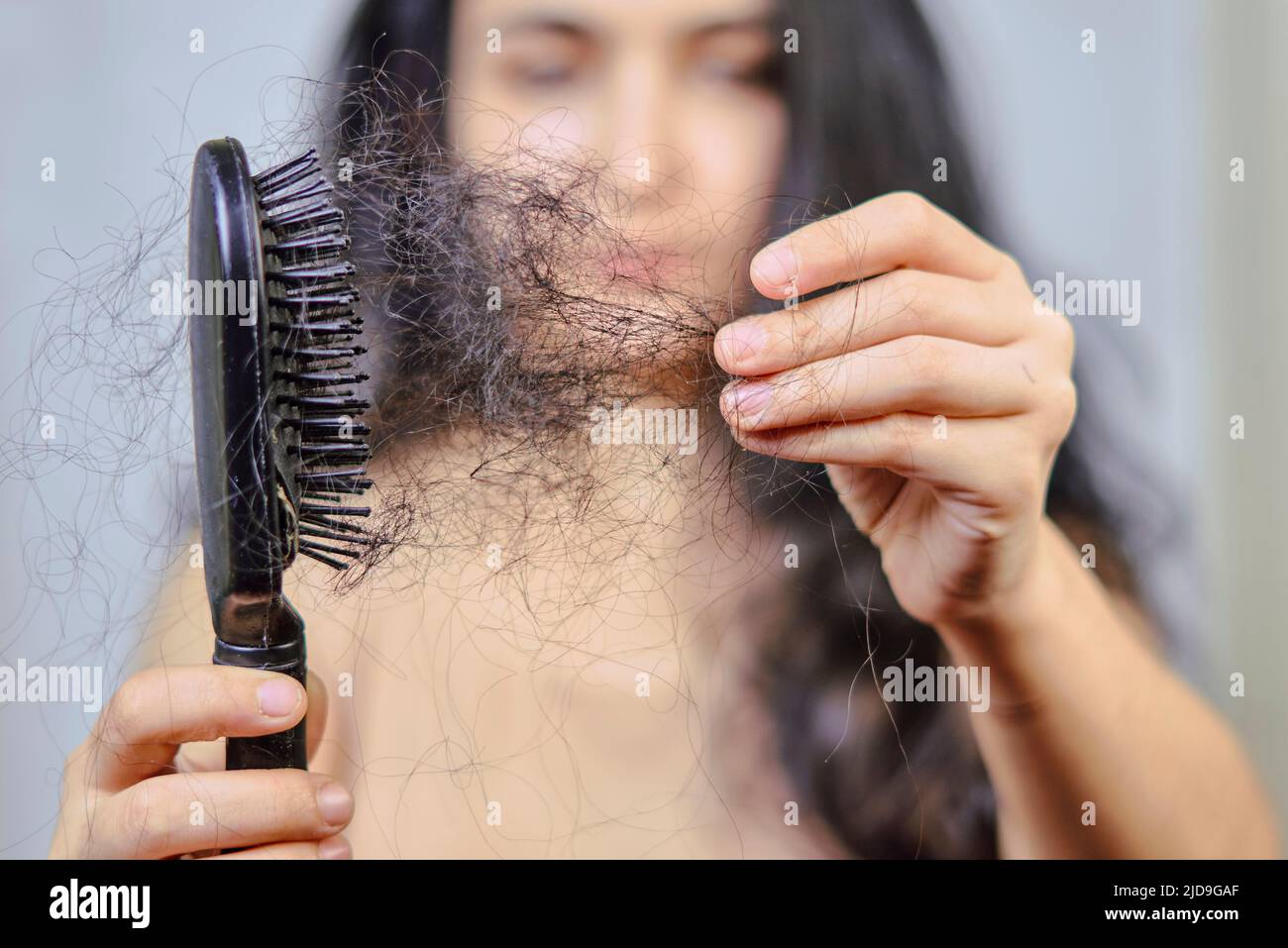
- Telogen Effluvium: A sudden, diffuse shedding of hair, often triggered by a significant physical or emotional stressor, pushing a large number of hairs prematurely into the resting phase. This type is frequently a symptom of an underlying health issue.
- Alopecia Areata: An autoimmune condition where the body’s immune system mistakenly attacks hair follicles, leading to patchy hair loss.
- Traction Alopecia: Hair loss caused by constant pulling or tension on the hair follicles from hairstyles.
While androgenetic alopecia is primarily genetic, many other forms of hair loss, particularly telogen effluvium and alopecia areata, are strongly linked to systemic health problems.
Hormonal Imbalances: A Major Culprit
Hormones play a critical role in regulating the hair growth cycle. Fluctuations or imbalances can significantly impact hair health.
1. Thyroid Disorders:
Both an underactive thyroid (hypothyroidism) and an overactive thyroid (hyperthyroidism) can cause diffuse hair thinning. Thyroid hormones are vital for metabolic processes, including hair follicle function.
- Hypothyroidism: Can lead to dry, brittle hair, diffuse thinning, and sometimes loss of the outer third of the eyebrows. Other symptoms include fatigue, weight gain, cold intolerance, and constipation.
- Hyperthyroidism: May result in fine, soft hair and diffuse thinning. Other symptoms include weight loss, rapid heartbeat, anxiety, and heat intolerance.
Proper diagnosis and treatment of thyroid dysfunction often lead to hair regrowth.
2. Androgen Imbalance (PCOS):
In women, elevated levels of androgens (male hormones) can lead to hair thinning, particularly on the scalp, mimicking male pattern baldness. Polycystic Ovary Syndrome (PCOS) is a common endocrine disorder characterized by hormonal imbalances, including excess androgen production. Women with PCOS may experience hair loss, acne, irregular periods, and hirsutism (excess body hair).
3. Pregnancy and Postpartum:
The hormonal shifts during pregnancy and after childbirth are a classic example of how hormones affect hair. Elevated estrogen levels during pregnancy often lead to thicker, fuller hair. However, a sharp drop in estrogen levels postpartum can trigger a significant shedding phase (postpartum telogen effluvium) as hair follicles rapidly enter the resting phase. This is usually temporary, with hair returning to normal within several months.
4. Menopause:
As women enter menopause, estrogen levels decline, which can lead to diffuse hair thinning and a reduction in hair density. The relative increase in androgen activity can also contribute to a pattern of hair loss similar to male pattern baldness.
Nutritional Deficiencies: Fueling Hair Growth
Hair follicles are among the most metabolically active cells in the body, requiring a steady supply of nutrients to support rapid growth. Deficiencies in essential vitamins, minerals, and proteins can severely impair hair production.
1. Iron Deficiency Anemia:
One of the most common causes of diffuse hair loss, particularly in women. Iron is crucial for producing ferritin, a protein that stores iron and is essential for hair cell proliferation. Low iron levels can prematurely push hair into the resting phase. Symptoms include fatigue, pale skin, shortness of breath, and brittle nails.
2. Zinc Deficiency:
Zinc plays a vital role in hair tissue growth and repair, as well as in the proper functioning of oil glands around the hair follicles. Deficiency can lead to hair loss, brittle nails, and impaired immune function.
3. Vitamin D Deficiency:
Vitamin D receptors are present in hair follicles, and studies suggest a link between low Vitamin D levels and various forms of hair loss, including telogen effluvium and alopecia areata.
4. Biotin Deficiency:
While rare in individuals with a balanced diet, biotin (Vitamin B7) is essential for healthy hair, skin, and nails. Severe deficiency can lead to hair loss.
5. Protein Malnutrition:
Hair is primarily composed of protein (keratin). Inadequate protein intake can lead to hair thinning and a dull appearance, as the body prioritizes protein for essential functions over hair growth.
6. Essential Fatty Acids:
Omega-3 and Omega-6 fatty acids are crucial for scalp health and hair shaft integrity. Deficiencies can lead to dry, brittle hair and a flaky scalp.
It’s important to note that self-supplementation without professional guidance can be harmful. Blood tests are necessary to confirm any deficiencies before starting supplementation.
Autoimmune Conditions: When the Body Attacks Itself
Autoimmune diseases occur when the body’s immune system mistakenly attacks its own healthy tissues. Several autoimmune conditions can directly or indirectly cause hair loss.
1. Alopecia Areata:
This is a classic example of an autoimmune disease directly targeting hair follicles. It results in patchy, non-scarring hair loss that can affect the scalp, beard, or any hair-bearing area. It can progress to total scalp hair loss (alopecia totalis) or complete body hair loss (alopecia universalis). Alopecia areata is often associated with other autoimmune conditions, such as thyroid disease, vitiligo, and lupus.
2. Systemic Lupus Erythematosus (SLE):
Lupus is a chronic inflammatory autoimmune disease that can affect various organs, including the skin and hair. Hair loss in lupus can be diffuse and non-scarring (telogen effluvium due to chronic illness) or specific to the scalp (discoid lupus erythematosus), which causes scarring alopecia and permanent hair loss in affected areas. Other symptoms include joint pain, fatigue, and a butterfly-shaped rash on the face.
3. Rheumatoid Arthritis (RA):
While not a direct cause, chronic inflammation associated with RA can contribute to telogen effluvium. Furthermore, some medications used to treat RA can have hair loss as a side effect.
Chronic Illnesses and Systemic Conditions
Many chronic diseases can impact hair health due to their systemic effects on the body.
1. Chronic Kidney Disease and Liver Disease:
These conditions can lead to nutrient deficiencies, hormonal imbalances, and the accumulation of toxins, all of which can contribute to diffuse hair thinning.
2. Diabetes:
Poor circulation, nerve damage, and chronic inflammation associated with uncontrolled diabetes can impair the delivery of nutrients to hair follicles, leading to hair loss.
3. Cancer and Cancer Treatments:
Chemotherapy and radiation therapy are well-known causes of hair loss, as these treatments target rapidly dividing cells, including hair follicle cells. While often dramatic, this hair loss is usually temporary.
4. Severe Infections:
Certain infections can cause hair loss. For example, secondary syphilis can cause a characteristic "moth-eaten" patchy hair loss. Fungal infections of the scalp (tinea capitis) can also lead to localized hair loss, often with scaling and inflammation.
5. Inflammatory Scalp Conditions:
Conditions like severe psoriasis or seborrheic dermatitis on the scalp can cause temporary hair loss due to intense inflammation, itching, and scratching, which damages hair follicles.
Medications and Their Side Effects
A wide array of prescription and over-the-counter medications can list hair loss as a potential side effect. This is often a dose-dependent effect and reversible upon discontinuation of the drug. Common culprits include:
- Anticoagulants (blood thinners): Warfarin, heparin.
- Antidepressants: SSRIs, tricyclic antidepressants.
- Blood Pressure Medications: Beta-blockers, ACE inhibitors.
- Cholesterol-lowering Drugs: Statins.
- Acne Medications: Isotretinoin (Accutane).
- Oral Contraceptives: Starting or stopping birth control pills can sometimes trigger telogen effluvium due to hormonal shifts.
- Chemotherapy drugs: As mentioned earlier.
It’s crucial to discuss any new hair loss with your doctor if you are on medication, but never stop a prescribed medication without medical advice.
Psychological Impact and Stress
The relationship between stress and hair loss is complex and often bidirectional. Severe physical or emotional stress can trigger telogen effluvium, leading to significant hair shedding several months after the stressful event. This can include:
- Major surgery or illness
- High fever
- Bereavement or emotional trauma
- Extreme dieting or sudden weight loss
Conversely, experiencing hair loss itself can be a significant source of psychological distress, leading to anxiety, depression, and a negative impact on self-esteem, which can, in turn, exacerbate hair loss, creating a vicious cycle.
When to Seek Medical Attention
While some hair shedding is normal, it’s important to consult a healthcare professional if you notice:
- Sudden or rapid hair loss.
- Patchy hair loss.
- Hair loss accompanied by other symptoms like fatigue, unexplained weight changes, skin rashes, joint pain, or changes in bowel habits.
- Scalp pain, itching, redness, or scaling.
- Hair loss in children.
Diagnosis and Treatment
A thorough medical evaluation is the first step in addressing hair loss. Your doctor will typically:
- Take a detailed medical history: Inquiring about your diet, lifestyle, medications, family history of hair loss, recent illnesses, and stress levels.
- Perform a physical examination: Including a close inspection of your scalp, hair, and other body systems for signs of underlying conditions.
- Order blood tests: These may include a complete blood count (CBC), iron studies (ferritin), thyroid function tests, hormone levels (e.g., testosterone), vitamin levels (e.g., Vitamin D, B12), and autoimmune markers (e.g., ANA).
- Consider a scalp biopsy: In some cases, a small sample of scalp tissue may be taken for microscopic examination, especially if a scarring alopecia is suspected.
Treatment for hair loss is highly dependent on the underlying cause. It may involve:
- Addressing nutritional deficiencies: Through dietary changes and targeted supplementation.
- Managing hormonal imbalances: With medication for thyroid disorders or PCOS.
- Treating autoimmune conditions: With immunosuppressants or other specific therapies.
- Adjusting medications: If a drug is identified as the cause.
- Managing stress: Through lifestyle changes, mindfulness, or therapy.
- Topical or oral medications: Such as minoxidil or finasteride, which can help stimulate hair growth in certain types of alopecia.
- Treating scalp conditions: With medicated shampoos or topical treatments.
Conclusion
Hair loss is far more than a cosmetic inconvenience; it is frequently a valuable diagnostic clue to underlying health issues. From hormonal imbalances and nutritional deficiencies to autoimmune diseases and chronic illnesses, the body often signals internal distress through changes in hair. Ignoring persistent or unexplained hair loss can mean missing an opportunity to diagnose and treat a potentially serious health condition.
By taking a holistic approach and seeking professional medical advice, individuals experiencing hair loss can not only address their hair concerns but also uncover and manage the root cause, leading to improved overall health and well-being.